Prevention of microbial contamination in pharmaceutical and biotech manufacturing areas: a holistic approach to establishing robust control measures.
A recent best seller1 tackled the question of why an entire nation can be compelled to help one or a few people in life-threatening situations (e.g. Chilean miners), but will do little to help millions who are at equal or greater risk (e.g. Tsunami victims). This may be irrational, but is also an accurate characterization of how difficult it is for humans to work toward abstract goals based on concepts and proportions that are frankly, nearly impossible to grasp. Saving one person, who is right in front of you, is far easier to conceptualize than saving millions who are suffering in a distant land. In situations such as these, the tendency is to turn away, because we cannot understand how to effect change to that which we cannot understand or see. This phenomenon plays a role in environmental control of drug manufacturing areas, in that, we are asking individuals who work in these areas to exercise a great deal of caution and to follow rigid protocols designed to prevent contamination of the drug by entities that number in the millions, that they cannot see. To put it simply, those who work in critical manufacturing areas have an innate tendency to underestimate the impact that they as individuals may have on controlling a large complex system, or on even more abstract concepts such as impacting the public health, which can be the outcome of poor manufacturing control, as evidenced by recent influenza vaccine shortages2 and product recalls3.
Effective management of drug manufacturing areas requires a holistic approach based on identifying and monitoring those components that play the most critical role in successful manufacturing outcomes. A holistic approach addresses behaviors of complex systems, based on a multi-disciplinary approach that relies heavily on metrics to understand the behavior of the system. The critical components that must be addressed and monitored in order to ensure drug production outcomes are: facility (design and condition), personnel (training and management) and microbial control programs (products and application). This article will address all three areas.
The best defense is a good offense, especially when there are millions of dollars and the public health at stake – which is not hyperbole when we are talking about vaccines and other biotechnology derived drugs. In this case, where terminal sterilization is typically not an option, a strong offensive position begins with a robust facility design that insulates the drug and packaging components from sources of contamination. This design includes adequate barriers (e.g. interlocking doors, clear zone demarcation), HVAC capacity (e.g. enough to handle seasonal fluctuations in temperature and humidity), water control (e.g. placement of drains and WFI drops), cleanable design features (e.g. smooth coving, limited obstructions) and selection of chemical and moisture resistant materials of construction (e.g. 316L stainless steel, epoxy or polymeric flooring), to name a few. In a situation with unlimited budget, time and expertise, design and construction of a drug manufacturing facility optimized to prevent product contamination can be easily achieved. However, in a less than optimized environment, the design and facility condition are often contributing factors to microbial excursions, and in some cases, to product contamination.
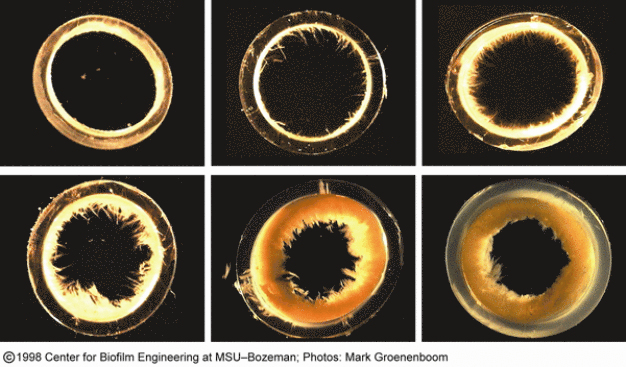
Even stainless steel may suffer the effects of chemical exposure, or over-exposure, resulting in rust. Rust and pitting, in particular, represent significant damage to the surface that present challenges to effective microbial control in two ways; one in providing shelter to microorganisms and residue, and two in inhibiting the cleaning and decontamination agents from reaching the microbes to achieve adequate contact time. Stainless steel is not the only surface that can be damaged; epoxy and polymeric floors can suffer significant damage from high foot traffic or the force of moving heavy equipment – and are not immune to the effects of significant chemical exposure. Both scenarios may lead to pooling water and the microbial control problems associated with water, such as mold and Bacillus proliferation. Significant water damage to the structure, as a result of, for example leaking roofs or drainage problems, can establish endemic problems with molds (see image 1) and Bacillus. Drainage issues, can result in biofilm (see image 2) formation, which may lead to significant, recurring problems with Bacillus and other bacteria due to increased resistance to antimicrobial chemistries demonstrated by biofilms4. Another aspect of design is inclusion of sufficient barriers to isolate the drug manufacturing process. Older facilities or facilities that were not originally designed for this purpose may not have an ideal barrier design. For example, the warehouse or component staging areas may not be ideally located to prevent egress of undesirable particulate. In some cases, one-way traffic cannot be established due to structural limitations. Both situations make contamination control more problematic and consequently, the drug manufacturing process more difficult to control.
The most common approach to microbial control problems due to facility design flaws or damage is to increase the use of chemical antimicrobial products, by concentration, frequency of application or both. In some cases, extremely aggressive chemical agents, such as acidified bleach, may be used on a shortterm basis. While these measures may result in immediate improvements in environmental monitoring data, in the long run, this approach may lead to even more damage and less ability to control the environment. The best solution to establish a high degree of control is to repair or retrofit the facility as required, a costly approach to be sure. However, it is less expensive than the alternatives of chasing root causes for microbial excursions or product contamination and rejection.
The personnel who work in aseptic manufacturing areas continue to represent the greatest threat to drug production. This is certainly not a reflection of the lack of dedication, because most people take great pride in doing a good job, but rather the inherent nature of humankind. Human beings are prodigious bioreactors; by some accounts5 90 percent of the cells on the human body are microbiological in nature. Further, even with robust training programs, the people who work in cleanrooms do not always adhere to good aseptic practices. The most common lapses in behavior have more to do with thoughtlessness, rather than willful disregard for aseptic practices. For example, one might thoughtlessly scratch an itch or mop a sweaty brow, or sneeze. Willful deviations from standard operating procedures may, in some cases, be meant to mitigate the risk of failing environmental monitoring data. For example, spraying sterile isopropyl alcohol on gloved hands or Tyvek suits immediately prior to plating, may reduce the risk of failing results, but is never condoned. Sometimes willful disregard for standard operating procedures and aseptic practices is more difficult to categorize. For example, during a training event years ago, an operator said that the reason she added an unapproved household dish detergent to the validated disinfectant solution to be used in the classified cleanroom was that she believed that the validated product did not produce enough foam, which she believed was essential to good cleaning (a fallacy that can be dispelled through training). In this situation, her intentions were noble, but her behavior was still non-compliant to cGMP practices. At the very least this placed her management in a poor regulatory situation, and in the worst case, her actions may have compromised the performance of the disinfectants, putting the drug at risk.
There are hundreds of ways that an aseptic environment can be compromised through the wellmeaning efforts of insufficiently trained and monitored personnel. The key to reducing operating risk from the personnel who work in these areas is to include a solid cGMP platform in the training program. This platform should draw on the evolving history of drug production, incorporating real-world examples of the damage that adulterated drugs represent to human health. Everyone knows someone who uses pharmaceuticals at least periodically (e.g. vaccines, chemotherapy); understanding what the risk of poor production control represents to a friend, loved one or to oneself, helps to personalize the message and drives more thoughtful behavior. Further, basic training in microbiology, antimicrobial chemistry and cleaning techniques, can ensure greater compliance by establishing a solid rationale for why certain products and conditions are used. In other words, through education, you are taking a large, complex system, which requires control of millions of non-visible objects, and scaling it to a level that the cleanroom operator can understand and embrace. Once this education is delivered, it must be reinforced through frequent management interaction. It is a sad fact of life that as operations management is asked to spend more time away from the manufacturing floor, there is less opportunity to observe behavior, which means there is less opportunity to reinforce the good and correct that which needs improvement. Further, as operations management becomes more involved in matters outside of their most basic function, personnel training and management, oversight problems may occur. “Specifically, no oversight to ensure that Shift Managers/Supervisors confirm employee completion of course requirements…Two current temporary employees were hired on…, but did not receive required training, SOP… “introduction to GMP”, as required by the firm’s training procedures.” GMP Trends, Inc. December 1, 2010.
Cleaning is a cGMP requirement. The environment must be controlled in order to prevent particulate and microbial contamination of the drug, packaging components, and product contact surfaces. The manner (e.g. products, application methods and frequency) in which cleaning and microbial control takes place varies from site to site, in part because of differences in facility design and production needs. However, there are guidance documents6,7 and best practices that should be incorporated into the cleaning and microbial control strategy. There are also practices that are not universally applied or sometimes well-understood. One such practice is disinfectant/sporicide rotation. The term itself has undergone change over the last decade or so. At one time, rotation implied alternating use of two broad-spectrum disinfectants of similar chemistry (e.g. two phenols, or two quaternary ammonium chloride (quats) compounds). By rotating two different formulations, with similar active ingredients and different chemical or physical properties (e.g. pH, alkalinity), one might address a broader spectrum of microorganisms (bacteria, fungi, viruses), while minimizing the development of problematic residues that may occur from the interaction of two different, and potentially incompatible chemical species (e.g. phenols and quats). At this time, the above type of rotation is still prevalent as evidenced by recent 483 observations, “The firm failed to follow written procedures for cleaning and disinfection of Class 10,000 rooms, in that, production personnel do not alternate cleaning and disinfection agents for sinks and flat surfaces, as dictated in SOP…” GMP Trends 8/15/07. However, as the need to control more resistant organisms, such as fungal spores and bacterial endospores, becomes greater, rotation programs are often refined to include the use of a sporicide. This model of alternating routine disinfectants, or one routine disinfectant, with a sporicidal agent, is fast becoming a regulatory preference, and is noted in various regulatory and advisory documents, including USP Disinfectants and Antiseptics, USP 32- NF27: “It is prudent to augment the daily use of a bactericidal disinfectant with weekly (or monthly) use of a sporicidal agent. The daily application of sporicidal agents is not generally favored because of their tendency to corrode equipment and because of the potential safety issues with chronic operator exposure. Other disinfection rotation schemes may be supported on the basis of a review of the historical environmental monitoring data.”
Selection of disinfectants and sporicides should be made based upon scientific evidence of efficacy against the target spectrum of organisms, as well as upon other important considerations such as substrate compatibility and operator safety. The references8 available to provide information on the mechanisms by which different chemical entities work against the structures of various microorganisms are too numerous to count. These tools can aid in the selection of disinfectants and sporicides. However, use of scientifically-based references and the conventional wisdom to select these products does not alleviate drug manufacturers of the requirement to validate their disinfectants and sporicides, and even isopropyl alcohol, for use in their facilities, against their environmental isolates, under actual use conditions. “Disinfectant agents used to sanitize surfaces in the aseptic processing areas (APA) have not been adequately qualified to assure that they provide the intended microbial decontamination when used in the manner as specified in the standard operating procedures as follows: a. The qualification study only evaluated stainless steel and not other surfaces in the APA such as glass, plastic and epoxy painted surfaces. b. The qualification study used a longer exposure time to the sanitizing agent then that time specified in the cleaning SOPs. c. The qualification study immersed the test surface in the disinfectant for ….. Instead of wiping the surface as specified in the SOPs.” GMP Trends May 1, 2003.
In addition to microbial efficacy, the question of the role that disinfectant and cleaning agent residues play in environmental control has become a more urgent concern. Most disinfectants and cleaning agents contain ingredients that are non-volatile,h i.e. remain on the surface once the volatile components evaporate. In many cases, these are inert substances; however, they can lead to visual and functional impact on surfaces (see image 3), and the impact of these residues should be evaluated with regard to subsequent cleaning and environmental monitoring activities. “No evaluation has been performed to ensure that cleaning solution residues do not negatively impact environmental sampling or testing.” Warning Letter, July 2, 2008. Therefore it is prudent to incorporate a rinsing strategy into your cleanroom contamination control procedures. This strategy should identify the rinsing agent, frequency of rinsing and specific application procedures. Further, if a rinsing agent other than purified water or isopropyl alcohol (i.e. products that leave no residues) is to be used then consideration must be made to the nature of the residues being introduced from the rinsing agent. Frequency of application needs to be considered on the basis of risk versus reward. Introduction of water or other rinsing agents too frequently, especially immediately following disinfection, may lead to even more microbial control challenges through dilution of the disinfectant before sufficient contact time is achieved for optimum performance or through the presence of too much water, a growth nutrient. Drug manufacturers face a variety of challenges. They must ensure that environmental monitoring data demonstrate a state of sufficient control to prevent adulteration of their product in an environment where the facility design, the personnel who work there, and the contamination control practices employed may contribute to the control challenges. A holistic approach, emphasizing the contribution of each part to the function of the entire complex system, is the best approach to attain the control that drug manufacturers require and that consumers deserve.
References:
1. Ariely, Dan 2010. The Upside of Irrationality, HarperCollins Publishers p237-256.
2. Roumeliotis, Gregory, 05 Jul 2006, FDA report sheds light on Chiron's problems. Outsourcing-Pharma.com
3. George, John, 17 January 2011, Another Johnson and Johnson Recall. Philadelphia Business Journal.
4. Donlan, Rodney M. Biofilms and Device-Associated Infections. Emerging Infectious Diseases Vol.7, No. 2, March-April 2001
5. Glausiusz, Josie, Your body is a Planet. Discover Magazine June 2007
6. United States Pharmacopeia, USP Disinfectants and Antiseptics, USP 32-NF27
7. EC Guidelines to Good Manufacturing Practice, Medicinal Products for Human and Veterinary Use, Annex 1, Manufacture of Sterile Medicinal Products, 25 November 2008 (rev.)
8. Block, Seymour S. 2001. Disinfection, Sterilization, and Preservation. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins p. 31-79
STERIS Deutschland GmbH
50933 Köln
Germany